What Treatments Are Available for Type 2 Diabetes?
One of the biggest contributing factors for the onset of type-2 diabetes is your lifestyle, but genetics may also determine if you are more susceptible to the disease. Therefore treatment that may work for someone else may not be the right one for you.
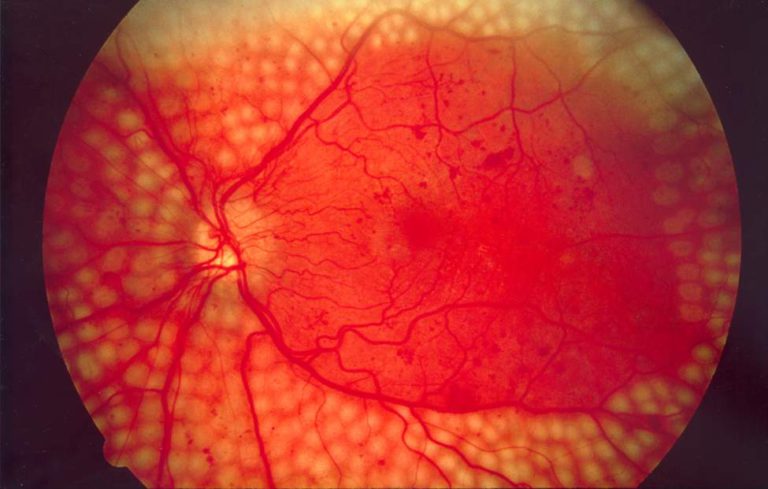
Successful management of type-2 diabetes involves targeting both glucose and non-glucose goals. Although glucose control is extremely important, the same amount of emphasis should be placed on achieving other health goals. For example, controlling hypertension (high blood pressure) can reduce the risk of complications such as retinopathy and neuropathy. Studies have shown that intensive glucose lowering did not reduce cardiovascular disease (CVD) related deaths, compared with standard glucose lowering. In fact, it could lead to a bigger risk of hypoglycemia and increased rate of hospitalization. Although tight blood sugar management may be more beneficial for newly diagnosed patients, it may be less effective for those with long standing type-2 diabetes.
Treatment choice and therapeutic targets should be individualized and based on clinical data as well as patient history, and all patients require a combination of non-pharmacological therapy and pharmacotherapy.
Treatment options
Diet and exercise have the greatest potential in stopping pre-diabetes converting into diabetes. In the Diabetes Prevention Program, these two factors decreased the onset of the disease by 58% after three years. The risk increases with bodyweight, and thus the first approach to the management of diabetes should be evaluating and altering your lifestyle.
According to clinicians, losing just 5-10 percent of your body weight can improve your blood sugar levels. Doing some form of exercise is essential – it does not have to be extreme, but can be something that you already enjoy doing such as walking or swimming. Combining cardio exercises with resistance training offers the most benefits than either activity alone. Try and break down 30 minutes of cardio exercise throughout the day, until you can do it for 30 minutes consecutively. It’s much easier when you are doing something you enjoy!
Food and dietary changes go hand in hand with exercise. Through individualized nutrition therapy, the patient and the healthcare provider can determine which diet would be best for you. In our previous blog post, we outlined some of trending diets for persons living with type-2 diabetes, which you can find here.
Sometimes it may be essential to treat diabetes with medicine. With pharmacotherapies, the goal of the treatment is to help your body use your insulin better. There are many different drugs available to help combat type-2 diabetes, but the most common first line of action is Metformin. The drug helps to improve insulin sensitivity by increasing peripheral glucose uptake and utilization. Dipeptidyl peptidase-4 (DPP-4) inhibitors may also be prescribed, which aim to lower high blood glucose levels without causing hypoglycemia (low blood sugar). Effectiveness of the drug is increased when paired with non-pharmacological therapy.
People with type-2 diabetes may need to take other medications for conditions related to diabetes, for example Diuretics to lower high blood pressure and it is important to always disclose this to a clinician as different drugs may be incompatible with each other. For best results, combining non drug and drug therapies is recommended, as often the underlying problem cannot be addressed by one approach.