14 Top Tips To Support Diabetic Eye Care
Here a few things every diabetes patient should know[1]:
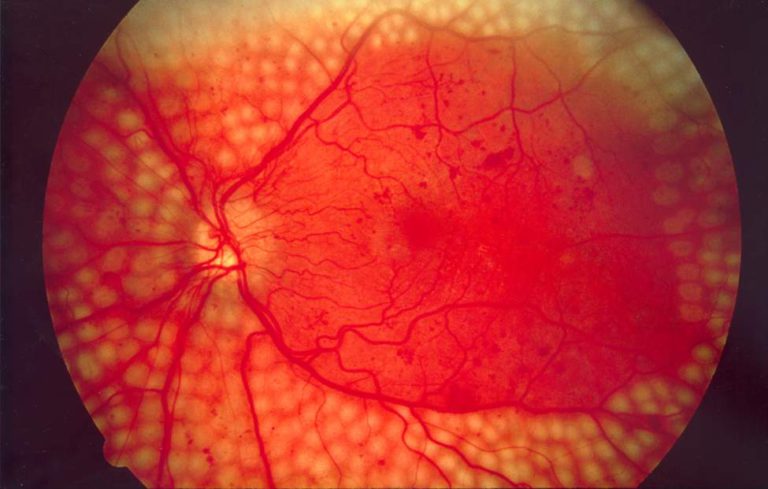
- Diabetes will eventually affect the blood vessels in your eyes. This is called diabetic retinopathy (DR), and it can lead to visual impairment and blindness.
- By controlling your blood sugar and blood pressure, you can reduce the damage diabetes can cause in your eyes. However, your eyes will eventually develop some diabetic changes. If you do get DR, it is not your fault.
- DR in most people has no symptoms — you cannot tell if you have it. Only an examination of the back of your eyes can find it. You should be examined every year.
- DR is treatable if it is found in the early stages. If you attend all your screening or clinic appointments, and have treatment when recommended, it is very unlikely that you will go blind.
- If you do not attend diabetic eye screening or eye clinic appointments, your DR can become very advanced and will affect your vision. If left untreated, you may go blind.
- Modern treatments with laser and drugs are very effective in stopping vision loss. However, treatment cannot restore vision that has already been lost.
Many factors feed into the challenges facing persons dealing with DR. These enabling and disabling factors include:
Patient beliefs
- Personal beliefs and attitudes towards diabetic eye disease are similar across the world and are best tackled through appropriately educating the patient.
- Eye care providers must play a key role in teaching patients about diabetic eye disease.
- Information about diabetic eye disease, screening, and treatment needs to be accurate, informative, and yet non-intimidating. It is better received when it is tailored to the individual: patients benefit from seeing the changes in their own retinal images, where this is possible.
Social attitudes
- In areas where social and cultural beliefs about diabetes or eye care services are detrimental to health seeking behavior, mass media or marketing campaigns may be the best strategy. Patients are most influenced by their family, so including family members in teaching sessions, consultations, and decisions is key to changing patients’ behavior.
- The purpose of retinal screening is to prevent loss of vision, particularly for those people who are less likely to seek out health services. Screening services therefore need to be made as accessible as possible.
- Common barriers for health professionals to address may include patient transport, clinic delays, limited and inconvenient timing of appointments, insufficient notice or publicity, intimidating health staff, and painful laser treatment.
- Patients will not attend diabetic eye care programs if they don’t understand why it’s important and when it’s appropriate. Health care providers therefore need to ensure that correct information about DR and its treatment is communicated effectively to the patient and their family.
- When patients come for screening, the experience should be as convenient, efficient, helpful, and painless as possible, to ensure that they continue their care.
Armed with this information, and using today’s technology, diabetic patients and vision care providers can overcome the obstacles to better self-care and improved patient outcomes. Regular screening is paramount.
The Retina Risk App empowers diabetic patients to become more involved in their health care decision-making. It supports patient self-management by showing the importance of regular eye examinations and seeking timely medical assistance. The App’s easy-to-visualize and effective patient education tools vividly demonstrate how improvement of modifiable risk factors (e.g., blood glucose, HbA1c, blood pressure) could significantly lower the risk of potentially blinding diabetic eye disease and expensive interventions.
The algorithm at the core of the Retina Risk (RR) App is based on extensive international research on risk factors known to affect the progression of DR, such as duration of diabetes, gender, blood pressure and blood glucose (HbA1c) levels. Clinical validation in 20,000 diabetics is robust and the results have been published in several respected medical journals.
[1] Thanks to ‘Community Eye Health’ (Sept 2011), UK International Centre for Eye Health https://www.ncbl.nlm.nih.gov/pmc/articles/PMS3218394/