Does Diabetes Cause Cognitive Problems?
The impact of diabetes on the brain, specifically on the cognitive functions of this vital organ such as memory and attention span, has been largely ignored and most of the focus of research has largely been on how this condition affects the kidneys, nerves, and eyes.
However, the latest studies have provided insights into the huge adverse impact that diabetes can create on the brain due to which people with diabetes may experience a faster cognitive decline.
The loss of cognitive functions of the brain can put people with diabetes at risk of neurodegenerative diseases even at a younger age. Hence, it is important to recognize and assess the diabetes-related cognitive problems to be able to adopt effective strategies to protect yourself from chronic neurodegenerative diseases such as dementia, Parkinson’s, and Alzheimer’s.
Read on to learn more about how diabetes causes cognitive decline and the effective ways to prevent it.
The alarming statistics related to diabetes and cognitive functions
According to the American Diabetes Association, cognitive decline and diabetes are more likely to coexist. It is estimated that nearly 25% of people above the age of 65 years have diabetes (both diagnosed and undiagnosed). Nearly 50% of people in this age group have pre-diabetes.
Studies have revealed that the increase in the blood sugar level caused due to diabetes in these patients can harm the brain cells in several ways due to which they may experience a decline in cognitive functions such as reduced memory and attention span and difficulty in maintaining focus.
Mild impairment of cognitive functions is often marked by language difficulties, forgetfulness, and other symptoms, which are noticeable but do not interfere with the routine tasks the patient has to perform. It is considered the state of transition between normal aging and the development of dementia or Alzheimer’s disease.
Researchers have also reported that these impairments in cognitive functions are more common in patients who have uncontrolled diabetes, especially with a history of earlier onset, greater severity, and longer duration.
The new findings have confirmed the results from previous clinical studies that suggested a strong association between uncontrolled diabetes and a decline in cognitive functions at a comparatively younger age.
Diabetes can also raise the risk of cardiovascular diseases, including a stroke that can allow cognitive dysfunctions more likely to occur.
The risk of mild to moderate cognitive impairment is more likely to affect patients who:
- Have developed diabetes before the age of 65 years
- Require regular insulin treatment
- Have had diabetes for longer than 10 years
- Have developed other complications due to this disease
There are several theories put forward to explain the link between diabetes and cognitive impairment. Let us have a look at the mechanisms that can contribute to the decline in cognitive functions in patients with diabetes.
Mechanism of cognitive decline in diabetic patients
Damage to the brain cells
Uncontrolled diabetes, both type 1 and type 2, is more likely to be the result of poorly controlled blood sugar levels. The persistently high blood sugar levels or the frequent fluctuations in the blood sugar levels can cause damage to the nerve cells called neurons in the brain leading to cognitive impairment as stated by this study.
The damage to these cells can trigger a process of inflammation due to the involvement of the immune cells. The immune cells, in turn, can release pro-inflammatory substances like cytokines that can trigger further damage to the brain cells.
Continued or chronic inflammation in the brain tissues in patients with long-term and uncontrolled diabetes can prevent the efficient healing of the inflamed cells due to which the cells may die. The irreversible damage to the brain cells followed by cell death is largely responsible for triggering the decline in cognitive functions.
As the brain continues to lose healthily and efficiently functioning cells, the ability of this organ to perform its functions is hampered.
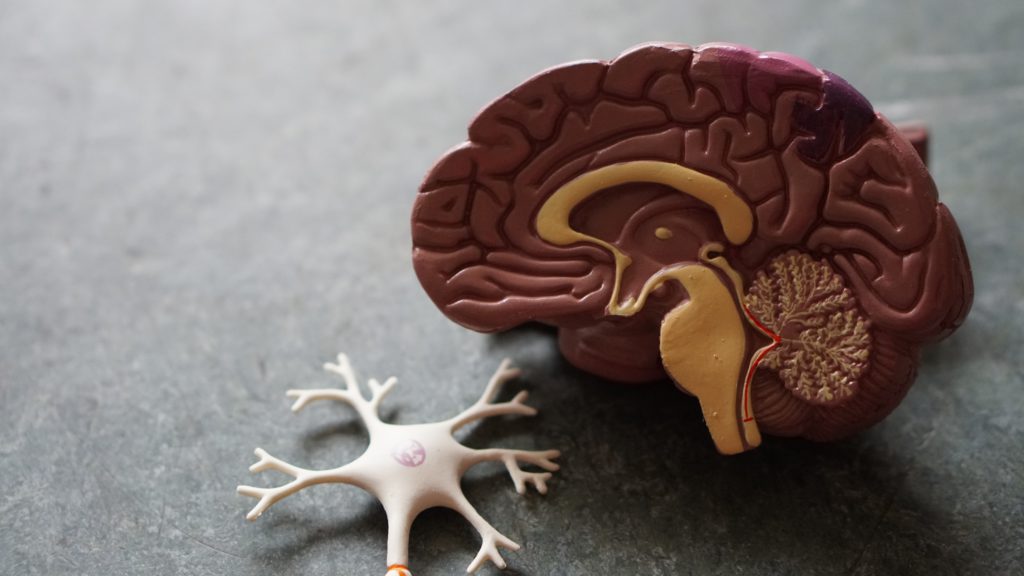
For example; the part of the brain that plays a role in processing new information related to the skills learned, and the names of people or places would no longer be as active and efficient as it should be.
Similarly, the functions of the brain cells involved in memory storage and recall will also be affected.
As a result of these changes, the patient would start experiencing difficulty in remembering names and places and lose the ability to learn new skills. This is how damage to the nerves due to uncontrolled or long-term diabetes can result in cognitive impairment.
Damage to the blood vessels
Diabetes-linked damage to the blood vessels that supply blood and other essential nutrients to the brain may also lead to the development of cognitive problems at a younger age.
Moreover, it has been found that patients with diabetic retinopathy, a common complication of diabetes known to affect the small blood vessels in the retina of the eyes, have a much higher risk of mild cognitive impairment. This supports the theory that the reduced blood supply to the brain cells can impair the functions of this organ just the way it affects the functions of the retina causing diabetic retinopathy.
Hence, patients with diabetes, especially those who are diagnosed with retinopathy, are advised to adopt healthy habits to control their blood sugar levels to prevent any serious complications like Parkinson’s and Alzheimer’s disease.
Inflammation
It is an important mechanism that is attributable to a higher risk of cognitive impairment in diabetic patients. We already discussed that chronic inflammation due to high blood sugar levels and cytokines released by immune cells could be responsible for triggering brain damage.
Inflammation may also occur due to insulin resistance in patients with type 2 diabetes. This form of diabetes occurs when the cells in the body are unable to respond to the hormone insulin produced in the pancreas. This state is called insulin resistance.
Insulin resistance can be the result as well as the cause of inflammation in the brain cells. This means the cells may develop resistance to insulin when they are inflamed due to the increased blood sugar levels.
At the same time, the reduced sensitivity of the cells to insulin can subject them to the repeated action of the hormone in an attempt to create the desired response. This means when a patient has insulin resistance, the blood sugar levels tend to remain high due to the inability of the hormone to work as expected. As a response to this, the pancreas produces more insulin in order to lower blood sugar levels. However, due to the already developed resistance, even the extra amount of insulin remains unutilized. But, this excess insulin subjects the cells to more damage due to which they can get inflamed.
This can trigger a vicious cycle due to which the damage to the brain cells continues to occur at a faster rate. This is how; insulin resistance can worsen inflammation and contribute to a faster cognitive decline.
Oxidative stress
Oxidative stress is another mechanism responsible for triggering the loss of cognitive functions in diabetic patients.
Diabetes is known to raise the risk of heart diseases like hypertension and myocardial infarction and cerebrovascular diseases like stroke. These diseases can cause damage to the heart and the blood vessels by worsening oxidative stress. The damaged blood vessels in the brain can lead to a faster cognitive decline.
Oxidative stress is the result of an increased release of free radicals in the body during metabolic processes. These free radicals can cause harm to the healthy tissues including the normal cells in the brain making them less efficient in performing their cognitive functions.
This marks the need to control your diabetes to be able to avoid the risk of hypertension, myocardial infarction, and stroke, which can otherwise lead to faster brain damage and cognitive impairment.
The effect of precursors
Type 2 diabetes is linked to a sedentary lifestyle, lack of exercise, and being overweight. These precursors of diabetes can also play a role in affecting brain functions.
Sedentary habits can further contribute to obesity due to which the patients may have more difficulties in controlling their blood sugar levels.
Moreover, the lack of exercise would lead to the accumulation of fats in the body. The fat cells are more prone to develop insulin resistance. So, the deposition of fatty tissues around healthy organs such as the brain could worsen insulin resistance making insulin less effective.
Additionally, the fat cells are also more likely to undergo inflammation and oxidative damage in the brain.
This is how the precursors to diabetes like the lack of exercise and obesity can make a person prone to develop cognitive decline.
Also, improper control of diabetes can cause too much glucose to remain in the blood. Over a period of time, this can cause damage to the organs, including the brain. Researchers are finding more evidence linking type 2 diabetes to a higher risk of Alzheimer’s disease, possibly due to the impact of obesity and other common precursors.
The lack of long-term control
Studies have found that the increase in the level of HbA1C, a parameter commonly used for evaluating diabetes control, can be responsible for causing damage to the brain cells.
HbA1C is one of the laboratory tests commonly recommended for diabetic patients. It involves drawing a sample of blood and testing it in a laboratory to measure the levels of a blood protein called glycosylated hemoglobin or simply hemoglobin A1C.
The early effect of diabetes on the brain can be correlated to the levels of HbA1C. Researchers have found that even patients who have had diabetes for less than ten years can develop deficits in memory functions that are typically associated with a part of the brain called the hippocampus. They have found that patients with diabetes usually have a smaller hippocampus than healthy people with normal blood sugar levels.
They have also discovered that the reduction in the size of the hippocampus is correlated to the increase in the HbA1C blood level, suggesting that the HbA1C test can be used to assess hippocampal functions and the onset of cognitive decline and memory loss.
Dysfunctions in the insulin pathway
Genetics plays a key role in insulin dysfunction. Research states that amyloid precursor protein genes are known to be involved in the pathogenesis of Alzheimer’s which have been found to affect the insulin pathways. Disruptions in this pathway are the characteristic signs of diabetes.
This indicates that an amyloid precursor protein gene can play a role in the development of both diabetes and Alzheimer’s disease providing an indirect link between these 2 conditions.
These findings suggest that a therapeutic approach that targets the insulin pathways by correcting the abnormalities linked to the amyloid precursor protein gene could help to control diabetes while also reducing the risk of Alzheimer’s.
Management of cognitive problems in patients with diabetes
There are several mechanisms through which diabetes can increase the risk of faster cognitive decline. It is important to identify these mechanisms and adopt ways to inhibit them to be able to prevent the loss of memory and other symptoms of cognitive impairment.
Optimum control of blood sugar levels through regular use of medications as prescribed by the physician, eating nutritious foods, and regular exercises can play a role in inhibiting or slowing down cognitive decline.
One of the challenges in managing patients with diabetes is the individualization of the treatment, especially when the patient is having multiple comorbid conditions.
Since microvascular and macrovascular complications of diabetes such as heart attacks, diabetic retinopathy, and stroke are well recognized, an attempt should be made to learn the best ways to avoid these complications.
Efforts should also be made to detect the dysfunctions related to the microvascular and macrovascular changes by checking the blood pressure, blood sugar levels, and heart functions on a regular basis.
Regular eye check-ups to assess the eyesight and the changes in the retina can also be helpful for detecting damage to the retina or macula. The early diagnosis of retinopathy can allow a patient to seek appropriate treatment aimed at preventing further loss of vision. It would also help him change the treatment protocol such that better glycemic control can be achieved in order to prevent other complications of diabetes like cognitive dysfunctions. Learn more about what causes diabetic macular edema here.
The aim of the treatment should be to detect the changes at the earliest through regular screening. Adopting these strategies would help patients minimize the impact of diabetes on their brain functions and protect them against the risk of cognitive impairment.
Conclusion
Diabetes and cognitive dysfunctions are highly prevalent disorders across the world. These conditions are also known to coexist and contribute to the worsening of each other.
Being aware of the risk of dysfunctions related to memory, attention span, focus, and concentration can enable diabetic patients to be watchful of the early signs and allow them to seek appropriate preventive and therapeutic measures to avoid them.