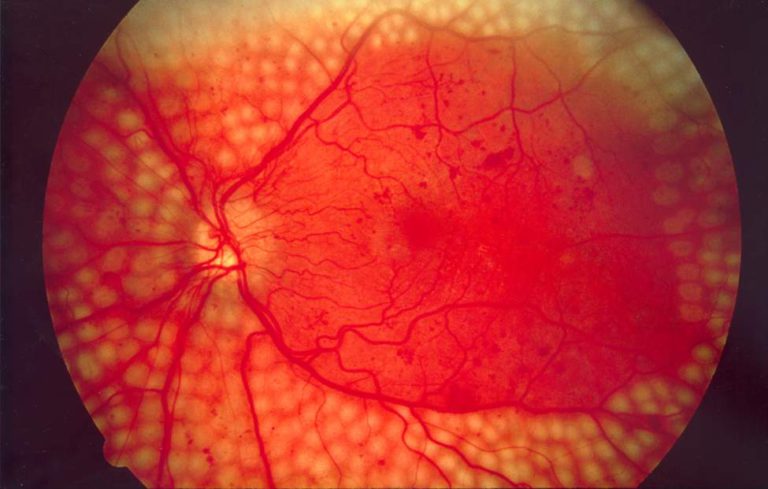
What is the Best Treatment For Diabetic Retinopathy?
Diabetic retinopathy is one of the most common complications caused by diabetes. If left untreated, it may affect the eyesight of the patient resulting in blindness. The latest scientific research studies have led to improved outcomes in the management of this condition. Below is a brief discussion about the latest treatments available to patients.
Below are some of the possible treatments for diabetic retinopathy
Lasers therapy
Laser treatment generally targets the damaged tissues of the eyes including the retina. Laser therapies offer more effective results in the management of retinopathies as the rays can directly work on the damaged retinal tissues through spot welding and photocoagulation. [1]
Laser therapies can also help to eliminate the abnormal blood vessels formed due to neovascularization. These treatments are recommended for patients with moderate to severe diabetic retinopathy. It can help to destroy the non-essential tissues along the periphery of the retina thereby reducing the production of VEGF (Vascular endothelial growth factor) and improving the blood supply to the central retina.
Laser therapy of the peripheral retina can allow blood to bypass this region and provide extra nourishment to the central part of the retina. Thus, the resulting boost in the supply of oxygen and nutrients helps to maintain cellular health in the macula, which plays a key role in supporting clarity of vision and color perception.
Depending on the specific symptoms and the extent of diabetic retinopathy, the ophthalmologist may advise patients to opt for grid laser or panretinal laser photocoagulation. [2]
Corticosteroid injections
Local injections of corticosteroids directly or in the forms of injectable implants are recommended for the treatment of more severe forms of diabetic retinopathies such as macular edema. In some cases, a combination of laser treatment and steroidal injections may be recommended.
Diabetic macular edema occurs when the diabetic retinopathy worsens due to the exposure to cytokines released by the immune cells. Cytokines cause inflammation in the retina thereby contributing to the pathogenesis of macular edema.
Steroidal injections and implants can offer better results in treating these complications by reducing the amount of VEGF and inflammatory cytokines produced by the immune cells through a process called “downregulation. [3]
It should be noted that the use of steroidal injections, anti-VEGF drugs, and implants has been approved by the FDA for the management of diabetic macular edema.
Surgical treatments
Patients diagnosed with proliferative diabetic retinopathy due to vitreous hemorrhage can achieve better results with surgical treatments like vitrectomy. Laser photocoagulation therapy is not suitable for these patients as the blood can obscure the view of the retina during surgery. [4]
Vitrectomy is recommended when vitreous hemorrhage fails to clear in a few weeks. The procedure includes the removal of the bloody vitreous and replacing it with a gel-like material. After vitrectomy, patients may undergo laser photocoagulation for faster recovery.
These advanced therapies can reduce the risk of formation of scar tissues that may otherwise cause traction on the retina leading to a retinal detachment.
Conclusion
Patients diagnosed with diabetes should visit an ophthalmologist regularly to assess the health of the eye, especially the retina. Early diagnosis of diabetic retinopathy and advanced therapies can improve the prognosis and reduce the risk of complications.
References:
- https://epub.ub.uni-muenchen.de/16401/1/10_1159_000098254.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4398802/
- https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3980167/