Anti-VEGF Injection Therapy For Patients With Diabetic Retinopathy
Ocular therapy using anti-vascular endothelial growth factor (VEGF) represents one of the most remarkable advances in modern medicine, especially related to the field of ophthalmology. The widespread and swift uptake of this therapy into clinical practice for the management of diabetic retinopathy and macular degeneration has helped to save the eyesight of millions of patients worldwide.
Recent studies have also revealed a decline in the incidence of blindness in patients with diabetic retinopathy and macular degeneration that is found to be coinciding with the increase in the use of anti-VEGF therapy.
Anti-VEGF therapy has provided a ray of hope to diabetic patients who are likely to develop complications like retinopathy and blindness. Here is a brief discussion of what exactly an anti-VEGF therapy means, how it works, possible side effects, and the role it can play in the management of diabetic retinopathy.
What is anti-VEGF therapy?
Anti-VEGF therapy refers to a group of medications that help to reduce the growth of new blood vessels through a process called neovascularization. This treatment can also be effective for reducing edema caused due to neovascularization.
Anti-VEGF medications can be used for the treatment of a number of eye disorders that involve the new blood vessel growth and swelling in the retina, especially in the macular region present at its center.
The growth of new, abnormal blood vessels at the macula can hamper the central vision due to which patients may experience problems while performing tasks like reading, recognizing faces, and watching television.
Anti-VEGF treatment can help to prevent neovascularization thus reducing these symptoms. It can also improve the central as well as peripheral vision affected due to diabetic retinopathy and macular edema, respectively.
However, anti-VEGF treatment has to be started at the earliest before or once the new blood vessels and swelling have begun to appear for deriving better outcomes. Initiating the Anti-VEGF treatment before there is excessive damage and swelling in the retina and macula is essential for minimizing the risk of loss of vision.
Importance of anti-VEGF drug in the management of diabetic retinopathy
Disorders of the arteries and veins supplying blood to the retina are responsible for triggering the most common causes of complete or partial loss of vision.
The disorders that can arise due to the damage to the blood vessels of the eyes include:
- Diabetic retinopathy, which is the most common precursor of blindness in the middle-aged population of most industrialized countries
- Retinopathy of prematurity, which is an important cause of blindness in pediatric patients, especially in the middle-income countries
- Age-related macular degeneration, which is the 3rd most common cause of blindness across the world
The development of these conditions is triggered partly due to the increased production of a protein known as VEGF or vascular endothelial growth factor. This protein plays a key role in the growth and development of new blood vessels.
VEGF production increases naturally in a state of hypoxia when the lack of an adequate amount of oxygen requires the body to produce new blood vessels in order to compensate for the reduced oxygen supply.
So, when a tissue is not receiving enough oxygen, it produces more VEGF, in an attempt to stimulate the growth and formation of additional blood vessels. It is one of the body’s own defense mechanisms that can be beneficial for preventing hypoxia of the heart muscles.
However, the same process can be harmful when it occurs in the eyes as increased secretion of VEGF could result in the steady progress of diabetic retinopathy.
The effect of VEGF in the eyes can be summarised as:
- Increased permeability of the existing blood vessels, thus causing them to leak fluids into the tissues of the eyes
- Growth of new blood vessels that may leak proteins and fluid or bleed
In the eyes, both of these effects can lead to serious retinal damage.
The normal retinal capillaries are usually sealed, thanks to the tight junctions present between the cells that form the capillary walls. This prevents the leakage of the larger molecules, like lipids and proteins, out of these capillaries into the macula or retina.
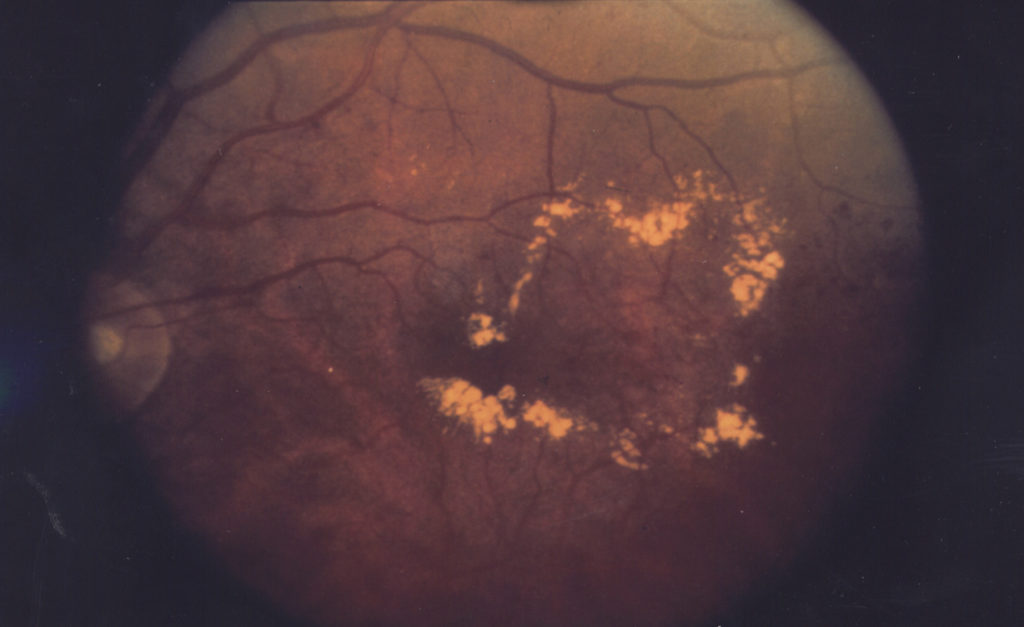
However, in the presence of an increased amount of VEGF, these capillaries begin to leak large molecules that form exudates, which later escape into the retina. This happens because the newly formed vessels are weak and fragile.
This leakage of fluid can result in edema and swelling in the surrounding tissue. When such changes occur in the macula, the central vision is reduced thus triggering the development of diabetic macular edema. We covered the causes of macular edema in-depth here.
The increase in the VEGF levels can also cause the growth of new retinal capillaries and blood vessels. However, these vessels are weak and abnormal. Also, they do not grow in the retina, where they might be useful for improving the blood supply to these tissues.
These abnormal capillaries, instead, tend to grow out from the retina and reach the surfaces of the vitreous. This can accelerate the progress of diabetic retinopathy and put the patient at risk of a more severe stage of this disease called proliferative diabetic retinopathy. To learn more on how diabetic retinopathy itself is diagnosed and treated, read more here.
Also, the new blood vessels are fragile and hence, prone to tearing. So, when a new blood vessel is torn or ruptured, it bleeds resulting in vitreous hemorrhage. This causes the vitreous to contract due to which the new vessels pull further on the retina, creating traction that leads to retinal detachment.
When the detachment involves the macula, the patient’s vision is impaired severely.
Moreover, in the presence of increased VEGF levels, new capillaries can grow out from the layer immediately below the retina called the choroid. These new blood vessels later grow into the spaces between the choroid and retina, usually just below the retinal pigment epithelium. These new vessels can leak exudates formed of blood and fluid, thus worsening the existing edema.
Eventually, a fibrous scar is formed at the site as a part of the body’s healing and repair mechanisms. However, the scar destroys the delicate photoreceptor cells present at the center of the macula thus contributing to the development of exudative AMD (age-related macular degeneration).
This suggests that the increase in the VEGF secretion can produce an adverse impact on the retina, macula, and other structures of the eye making patients vulnerable to develop diabetic retinopathy and other diseases that can eventually lead to partial or complete blindness.
This marks the importance of anti-VEGF treatment to inhibit the effect of VEGF and prevent the chain of events responsible for causing blindness in a vulnerable group of patients, especially those who suffer from diabetes.
Which are the most commonly used Anti-VEGF drugs?
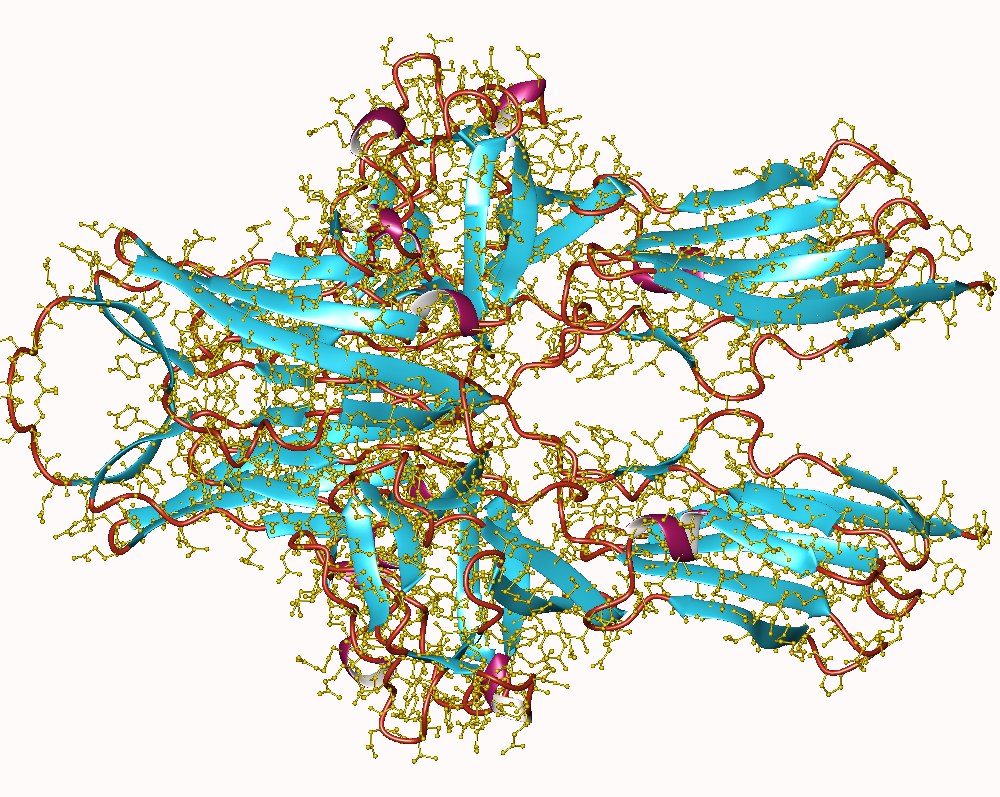
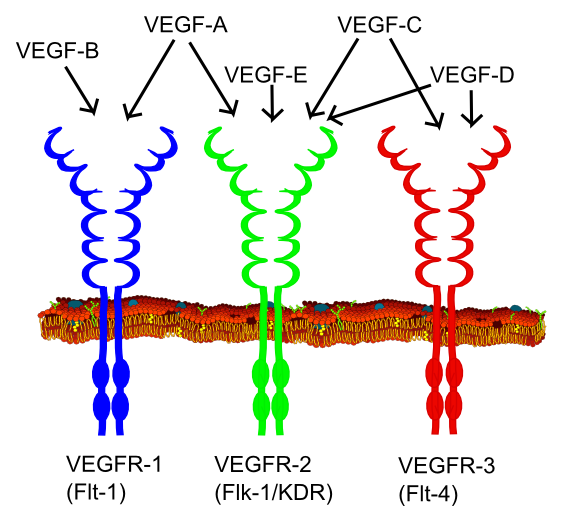
The two widely used Anti-VEGF drugs at present are ranibizumab and bevacizumab. These are monoclonal antibodies, which have the ability to bind to all 3 forms of VEGF.
Both of these are similar drugs in terms of their mechanism of action, though ranibizumab has a smaller molecular size and an ability to bind to VEGF in the eyes with a higher affinity. Ranibizumab is also purely intended for intraocular therapy, with each vial meant to be used only for 1 patient.
Bevacizumab, on the other hand, is administered intravenously for the treatment of cancer as well. It is an effective anti-cancer drug that comes in vials having multiple doses.
Aflibercept is another medication used for the treatment of diabetic retinopathy and wet macular degeneration. It is also an effective VEGF inhibitor that works by acting as a decoy receptor, which binds to the VEGF receptors on the endothelial cells in the walls of the blood vessels. It causes an inhibition of the activation of endothelial cells thereby preventing the formation of new blood vessels in the retina and macula.
Which eye conditions can be treated with anti-VEGF injections?
Other than diabetic retinopathy, anti-VEGF treatment is recommended for the treatment of other eye conditions such as:
- Macular edema
- Age-related macular degeneration
- Myopic choroidal neovascularization
- Macular edema caused due to retinal vein occlusion
How do anti-VEGF injections work?
Once anti-VEGF medications are injected into the eyes, they bind to the VEGF preventing it from interacting with the endothelial receptor sites. This action helps to stop or slow down the extra vessel growth and blood vessel leakage thereby preventing the progress of diabetic retinopathy and reducing the risk of blindness. If you are interested in other retinal diseases, we covered them and the treatments in this post.
Anti-VEGF treatment protocol for diabetic retinopathy
Regardless of the indication, the treatment using anti-VEGF injections for patients with retinal or macular disorders essentially involves two regimes:
- Continuous anti-VEGF treatment
- Intermittent (or as required) anti-VEGF treatment
Most initial trials aimed at assessing the benefits of anti-VEGF treatment were performed as a continuous protocol that involved regular monthly injections of these drugs over a course of two years.
This regimen involves 24 anti-VEGF injections that are administered into the eye once a month. However, this protocol can be inconvenient and expensive for patients as it requires them to visit the ophthalmologist more frequently.
The intermittent anti-VEGF treatment usually consists of 3 injections given over a period of three months, followed by the evaluation of the response to the treatment.
If there is an improvement in the symptoms supported by a reduction in the swelling in the retina, no additional treatment is needed.
If patients have some improvement in the symptoms, it would justify continuing the treatment further with anti-VEGF injections.
However, if there is no improvement at all, further treatment may be deemed futile. In this case, alternative treatments may have to be planned to prevent further loss of vision.

Also, it should be noted that even the patients, who have experienced an improvement in the symptoms with the initial 3 injections, may have relapses and require further treatment in the future. Hence, patients must be reviewed regularly in the clinic every 1 to 2 months.
During the follow-ups, testing of the retinal thickness and visual acuity is performed to assess the need for re-starting the treatment with anti-VEGF injections. If the visual acuity of the patient is lower by 1 or more lines, or if macular edema is found to be worse, further injections may be recommended.
What to expect during anti-VEGF treatment
The anti-VEGF treatment for diabetic retinopathy usually takes place in the doctor’s office.
Your doctor will put anesthetic drops into the affected eye to ensure you do not feel pain during the procedure. He will also clean the surface of the eye to prevent contamination and the risk of infections.
Then, he will apply a device to hold the eyelids open and administer the injection into the eye using a fine needle.
You might feel mild discomfort and pressure during the procedure. You may also experience visual disturbances as the fluid in the eye mixes with the injected fluid.
What to expect after anti-VEGF treatment?
After the treatment, your doctor will clean the area around the eye and examine it. The use of antibiotic eye drops and other medications may also be recommended to prevent infections and relieve pain.
You may experience mild side effects like blurred vision, soreness, and the appearance of floaters in front of the eyes.
However, these symptoms are usually mild and tend to disappear in 2 or 3 days.
Side effects of anti-VEGF therapy
VEGF can produce an effect on all the organs of the body by modifying the processes involved in the formation of new blood vessels. Hence, anti-VEGF drugs for the treatment of diabetic retinopathy have to be administered through a route that produces a local effect only in the eyes, without any adverse effect on the other parts of the body. In clinical practice, this means the drug must be injected directly into the eye through intraocular injections.
However, this mode of administration carries a higher risk of side effects like infections. It has been found that 1 in every 1000 anti-VEGF injections involve serious complications like infections, cataracts, retinal detachment, and vitreous hemorrhage.
Hence, these injections must be handled carefully and administered with appropriate aseptic techniques by an expert ophthalmologist in order to improve the outcomes and minimize the risk of side effects.
Some other possible side effects of this therapy include:
- A small bleed at the site where the needle was inserted
- Blurring of vision
- Pain or redness in the eyes
- Feeling as if there is something in the eye
- Appearance of floaters in front of the eyes
- Increased pressure inside the eye
- Increased sensitivity to light
Severe complications, like retinal detachment or tear, are rare.
What is the expected prognosis or success rate of anti-VEGF therapy?
Anti-VEGF therapy is highly successful for preventing vision loss related to diabetic retinopathy and macular degeneration. Studies have shown that nearly 90% of patients experience the stabilization of vision after this therapy.
Patients may also regain some lost vision if the treatment is started early before there is serious damage to the macula or retina.
Conclusion
Anti-VEGF drugs are highly effective for the treatment of diabetic retinopathy. These medications can also be included in the treatment regimen of other eye conditions like macular edema, and macular degeneration.
Though anti-VEGF drugs do not eliminate the underlying cause, repeated treatments could help to minimize the consequences linked to the same. It would help to prevent the risk of complete vision loss and even enable the restoration of vision to some extent.
Anti-VEGF drugs are expected to play a promising role in the prevention of blindness in diabetic patients. As the population across the world ages, and becomes more obese, the incidence of diabetic retinopathy is feared to worsen sharply.
However, regular monitoring of diabetes and eyesight, as well as the early diagnosis and intervention with anti-VEGF drugs might help to control the risk of blindness in vulnerable patients.